Scotland's Maternity Meltdown - A National Betrayal of Mothers and Families
11th December 2025
Scotland is facing a maternity crisis that stretches from its largest cities to its most fragile rural communities.
What should be the most basic promise of a modern health service — safe, accessible care for mothers and newborns has been undermined by delays, downgrades, staffing shortages, and broken promises. The result is a system that leaves families anxious, communities hollowed out, and Scotland's birth rate at historic lows.
Scotland's fertility rate has fallen to 1.3 children per woman, far below replacement level. In 2024, fewer than 45,000 babies were born which is the lowest number on record. Economic pressures and social change play a role, but maternity service failures amplify the decline. Families in rural areas openly say they will not have more children, or they relocate to safer regions. Poor maternity provision is not just a health issue and it is a population sustainability crisis.
Aberdeen - The Hospital That Never Arrives
The Baird Family Hospital in Aberdeen was meant to be a flagship centre for maternity, neonatal, and women's health services. Approved in 2014 with an opening target of 2020, it has become a symbol of failure. Construction did not begin until 2021, and repeated design flaws, remedial works, and pandemic disruptions have pushed the opening back to 2027 — seven years late and £100 million over budget. In the meantime, families are left with outdated facilities and a sense of betrayal. Can it get any worse - well think ferries!!!!
Edinburgh - A Culture of Mistrust
At the Royal Infirmary of Edinburgh, inspections in 2025 revealed a "culture of mistrust" and unsafe staffing levels. Healthcare Improvement Scotland identified 26 areas where standards were not met, including overstretched midwives and poor staff support. For a capital city hospital to be failing mothers so profoundly is a damning indictment of leadership and planning.
Elgin - Dr Gray's Downgrade
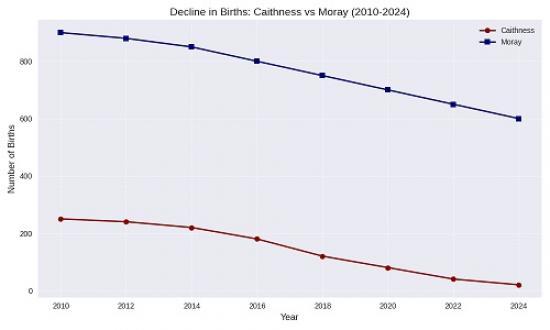
Moray's Dr Gray's Hospital lost consultant‑led maternity care in 2018, forcing mothers to travel long distances to Aberdeen or Inverness. Community anger has been fierce, with campaigners demanding restoration of full services. A recruitment drive has filled most posts, and the government promises consultant‑led care will return by 2026. Yet years of neglect have already discouraged young families from settling in Moray, contributing to stagnating population growth.
Wick - Caithness General's Baby Drain
Caithness General Hospital was downgraded in 2016, leaving only midwife‑led care. Mothers now face 100‑mile journeys to Inverness, often in ambulances, to give birth. Birth numbers in Wick have collapsed to fewer than 20 per year, compared to hundreds before the downgrade. Campaigners describe this as a "new Highland Clearances," with young families leaving the region rather than risk unsafe maternity provision. The demographic consequences are stark: Caithness is losing its future generation.
Inverness - Raigmore Under Strain
Raigmore Hospital in Inverness has become the reluctant hub, absorbing demand from Caithness and Moray. A £9 million extension was approved in 2024, but funding pressures have raised doubts about delivery. Raigmore's growth contrasts with the decline of surrounding areas, showing how centralization of maternity care reshapes population patterns.
National Consequences: Scotland's Birth Rate Collapse
Scotland’s fertility rate has fallen to 1.3 children per woman, far below replacement level. In 2024, fewer than 45,000 babies were born — the lowest number on record. Economic pressures and social change play a role, but maternity service failures amplify the decline. Families in rural areas openly say they will not have more children, or they relocate to safer regions. Poor maternity provision is not just a health issue; it is a population sustainability crisis.
A Systemic Failure
The Royal College of Midwives has warned of chronic staffing shortages across Scotland. Baroness Amos’ national review in 2025 confirmed that maternity failings are systemic, not isolated. From Edinburgh’s unsafe staffing to Aberdeen’s endless delays, from Moray’s broken promises to Caithness’s baby drain, the picture is one of a nation failing its mothers.
A Betrayal That Demands Action
Scotland’s maternity services are collapsing under the weight of mismanagement, underinvestment, and neglect. Families are forced into long journeys, outdated wards, and unsafe staffing levels. Communities are losing young people and future generations. The government’s promises of reviews and recruitment drives ring hollow against the lived reality of mothers denied safe, local care.
This is not just a healthcare issue — it is a national betrayal. Unless Scotland confronts its maternity meltdown with urgency and honesty, the consequences will echo for generations, in declining birth rates, hollowed‑out communities, and a broken trust between families and the health service that should protect them.
Businesses May Have Concerns Especially In Rural Areas
Why Health & Maternity Services Matter for Business
Workforce attraction and retention: Companies need skilled workers. If young families avoid areas with downgraded maternity units (like Caithness or Moray), businesses struggle to recruit and retain staff.
Community sustainability: Businesses depend on stable populations. Declining birth rates and outward migration in areas with poor maternity provision weaken the long‑term customer base and workforce pipeline.
Reputation and wellbeing: Employers increasingly emphasize employee wellbeing. Locating in areas where families feel unsafe about healthcare can undermine corporate responsibility goals.
Infrastructure signals: Delayed projects like Aberdeen’s Baird Family Hospital send negative signals about public investment reliability, which businesses factor into risk assessments.
Evidence & Reports
The Royal College of Nursing highlighted that healthcare gaps in rural Scotland create challenges for both residents and employers, noting that workforce strategies must address health access to sustain communities.
The Royal College of Midwives argued that investing in maternity services is also an investment in Scotland’s future workforce, warning that shortages risk undermining economic growth.
Research on maternity care in rural Scotland found that families weigh healthcare access heavily when deciding where to live, which directly affects local demographics and business viability.
The National Centre for Remote and Rural Health and Care has linked sustainable healthcare provision to broader rural development strategies, emphasizing that health services are part of the infrastructure businesses rely on.
Risks for Businesses
Recruitment difficulties: Skilled workers may refuse relocation if healthcare is inadequate.
Population decline: Fewer young families means shrinking markets and talent pools.
Community pushback: Businesses seen as ignoring local health concerns may face reputational damage.
Economic fragility: Poor services can accelerate depopulation, undermining long‑term investment returns.
Businesses do consider health and maternity facilities when locating in rural Scotland — not always as a primary factor, but as part of the wider picture of workforce sustainability and community viability. Weak maternity provision contributes to depopulation, which makes rural areas less attractive for long‑term investment.
Scottish Government
A masterclass in kicking the problem into touch.
The Scottish Government’s new national review of maternity services was formally announced in November 2025. It is expected to begin in early 2026, with the first findings and recommendations due later that year. A full report is anticipated in 2027.
Timeline of the Review
November 2025:
Public Health Minister Jenni Minto confirmed the review after pressure from MSPs and campaign groups.
The Royal College of Midwives (RCM) welcomed the announcement but warned against further delays.
Early 2026:
The newly established Scottish Maternity and Neonatal Taskforce will set the scope and begin work.
Evidence gathering from NHS boards, staff, and community groups will start.
Late 2026:
Interim findings are expected, focusing on urgent staffing and safety issues.
The government has promised "actionable recommendations" rather than just consultation.
2027:
A full national report is scheduled, covering maternity service design, delivery, and rural provision.
This will feed into long‑term planning alongside the Best Start framework, which reported in May 2025 on earlier reforms.
The review will start in early 2026, with interim findings later that year and a full report in 2027. Campaigners are pressing for urgent action, fearing that Scotland’s maternity crisis cannot wait for another slow process.
Don't forget some campaigns have been here before - Caithness under North Action Group was in action back in 2004.
So..............
